SATuRN and BioAfrica open access reports:
Here we provide you with sections from our open access annual reports, which are directed at public health practitioners, policies makers, doctors, researchers and the general public.
The objective of these reports is to present the key aspects of our work in an accessible, summarized format. The majority of the work presented has been published in peer-reviewed publications and can be seen in the publications section of krisp.org.za.
Phenotypic Resistance to Etravirine in an HIV-1 Subtype-C Background
Authors: AE Basson, S-Y Rhee, CM Parry, T de Oliveira, D Pillay, R Shafer and L Morris�
Background:
South Africa has an estimated 5.7 million people infected with HIV-1 of whom 919,923 were receiving antiretroviral treatment by the end of 2009. The first-line regimen includes a non-nucleoside reverse transcriptase inhibitor (NNRTI), either efavirenz or nevirapine. Both drugs share similar mutation profiles and exhibit cross-resistance. Here we examine the phenotypic sensitivity of single and double NNRTI mutations found in patients failing either nevirapine or efavirenz, to a second generation NNRTI, etravirine which has an unrelated resistance profile.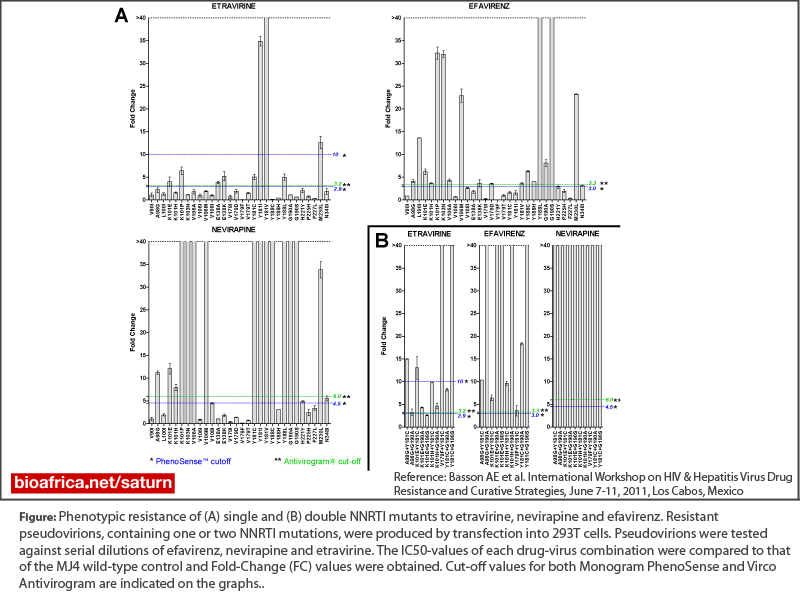
Methods:
Single and double NNRTI resistance mutations were introduced into an HIV-1 expression plasmid containing a ~3.7 kilo-base gag-pol insert from a subtype-C reference strain. The NNRTI mutation list from the International AIDS Society was used for selection of single mutants. Double mutants with significant covariation were identified by performing a Jaccard analysis on sequences from NNRTI experienced patients. Mutant plasmids were transfected into 293T-cells for the production of HIV-1 resistance vectors, and used to infect 293T-cells in serial dilutions of efavirenz, nevirapine and etravirine. Fold-change (FC) values were deduced for each virus-drug combination. Phenotypic resistance was classified by use of the Monogram PhenoSense and Virco Antivirogram cut-off values.�
Results:
Of the 30 single NNRTI mutations tested, only Y181I (FC>40) and Y181V (FC>40) caused high level resistance to etravirine. Mutations K101E/P, E138A/K, Y181C, Y188L and M230L gave a low to intermediate level of resistance. Mutations K101P, K103N, V106M, Y188L, G190S and M230L caused high-level resistance to efavirenz and nevirapine, while Y181C/I/V, Y188C/L and G190S conferred high-level resistance to nevirapine only. Mutation V179F conferred hyper-susceptibility to all three NNRTIs (FC=0.004-0.151). Mutation Y188C, although conferring high level resistance to nevirapine (FC>40), conferred hypersusceptibility to etravirine (FC=0.144). All eight double mutations caused high-level resistance to nevirapine (FC>40), and some to efavirenz. Interestingly, the combination of V179F with Y181C caused a high level of resistance to both etravirine (FC=>40) and nevirapine (FC>40). The Y181C and G190S double mutant was the only other combination that caused high-level resistance to etravirine (FC>40).Conclusion:
NNRTI resistance mutations, either singly or in combination, that arise in response to nevirapine or efavirenz rarely conferred high levels of resistance to etravirine. However, the combinations of V179F/Y181C and G190S/Y188C conferred high level resistance to ETV, as has previously been predicted. As combinations are not prevalent in currently failing individuals, etravirine is a suitable option for first-line NNRTI-based regimen salvage.Latest Reports
KRISP has been created by the coordinated effort of the University of KwaZulu-Natal (UKZN), the Technology Innovation Agency (TIA) and the South African Medical Research Countil (SAMRC).
Location: K-RITH Tower Building
Nelson R Mandela School of Medicine, UKZN
719 Umbilo Road, Durban, South Africa.
Director: Prof. Tulio de Oliveira




